An Overview of Amyloidosis, a Potential Cause of COVID-19 Complications and Vaccine Adverse Events
Amyloidosis is associated with clots, heart failure, nervous system issues, lungs with ground glass, acute myocarditis, taste loss, etc...
“SARS-CoV-2 infection is associated with a surprising number of morbidities. Uncanny similarities with amyloid-disease associated blood coagulation and fibrinolytic disturbances together with neurologic and cardiac problems led us to investigate the amyloidogenicity of the SARS-CoV-2 spike protein (S-protein).”
Journal of the American Chemical Society:Amyloidogenesis of SARS-CoV-2 Spike Protein
“A Swedish group showed that certain peptides in the spike can form amyloid strands”
Nature: Could tiny blood clots cause long COVID’s puzzling symptoms?
Amyloidosis is a group of diseases caused by the buildup of misfolded proteins. It is a strong candidate to be the causal link between the SARS-CoV-2 virus, and some of the unusual complications seen in both COVID-19, and vaccine adverse events. Amyloidosis is associated with clots, nervous system issues, heart failure, lungs with ground glass, acute myocarditis, taste loss, and many other issues. These are not normal complications of respiratory infections, yet they are occurring in patients with COVID-19.
The number of papers which support this connection is substantial, but there is a near total absence of it as a topic in the discussion around COVID-19 and vaccine adverse events. It has remained under the radar of not just the public, but those dedicated to investigating these issues. After a review of the data, I am shocked that more experts did not bring this forward to be a part of the general conversation in early 2020.
As I am not an expert, this post is not meant to be a summary. It is designed to give readers a general awareness that the connection exists, as well as starting point for understanding the components that the broader discussion involves. Included upfront are links to several papers connecting amyloidosis and COVID-19. There is a series of context based definitions for the most important vocabulary, meant to be read in order. Finally there is a sampling of the papers showing the general association of amyloidosis with specific issues, and links to articles covering the connection between SARS-CoV-2 and amyloidosis.
SAR-CoV-2 and Amyloids
SARS-CoV-2 infection can increase the body's production of amyloids.123456789
SARS-CoV-2 viral proteins are prone to forming amyloids.10111213
Spike protein subunit S1 is known to cross the blood brain barrier.14151617
Spike protein subunit S1 is linked to amyloid formation in the brain.181920
COVID-19 linked to persistent amyloid in the brain.2122232425
Amyloids detected in patients with 'long' COVID-19.2627282930
SARS-CoV-2 Spike has Prion-Like Domains (Self Replicating Amyloid).31323334353637
SARS-CoV-2 Vaccination Site Contains Amyloids38.
Amyloidosis is group of diseases caused by the build up of amyloids.
Amyloids are fibrils of misfolded proteins.
Fibrils are chains of molecules, with diameters of 10-100 nanometers. They are insoluble, resistant to degradation, and prone to clotting.
Prions are misfolded proteins that can transmit, misfold properly folded proteins.
Proteins are chains of amino acids. They make up most cellular structure.
Ribosomes are structures within cells which create protein chains.
Translation is the process of ribosomes creating proteins chains from mRNA.
Folding is the process of protein chains forming 3 dimensional structures. It can consist of several stages where multiple protein subunits form a protein complex.
Protein Subunits are protein molecules intended to be part of a protein complex.
Protein Complexes are groups of multiple proteins. They are the structures which enable most high level biological interactions to occur.
Protein Structure determines the behavior of a protein.
Antibody Related Amyloidosis
Antibodies are protein complexes with 4 protein subunits, 2 heavy chains, and 2 light chains.
Light Chains are antibody protein subunits, classified as kappa (κ) or lambda (λ).
Serum Free Light Chains (SFLC/FLC) are unbound light chain subunits in your blood. The counts, as well as ratio, of kappa (κ) and lambda (λ) proteins, are measured in SFLC/FLC tests.
Light Chain Amyloidosis is when misfolded light chain subunits of antibodies form fibrils that build up to levels which cause disease. It is also known as Primary Amyloidosis, and AL (amyloid light chain) Amyloidosis. Light Chain Amyloidosis is the most common form of amyloidosis.
Inflammation and Lipid Related Amyloidosis
Acute-phase Proteins are proteins whose production changes with inflammation.
Apolipoproteins are proteins which carry lipids.
Serum Amyloid A (SAA) is an acute-phase apolipoprotein.
AA Amyloidosis is when misfolded AA subunits of the lipid carrying protein serum amyloid A (SAA) forms fibrils that build up to levels which cause disease. It usually occurs as a complication of an inflammatory disease. It is also known as Secondary Amyloidosis. AA Amyloidosis is the second most common form of amyloidosis.
Cytokines and Interleukin 6 (IL-6)
Cytokines are proteins used to signal a cell response.
Interleukins are a group of cytokines related to the immune system.
Interleukin 6 (IL-6) is an interleukin often produced by blood vessels to signal a pro-inflammatory response, but it has many roles. It is known as B-cell stimulatory factor-2 (BSF-2), as it stimulates the production of antibodies. It also increases the production of Serum Amyloid A. High IL-6 levels are a marker for severe COVID.
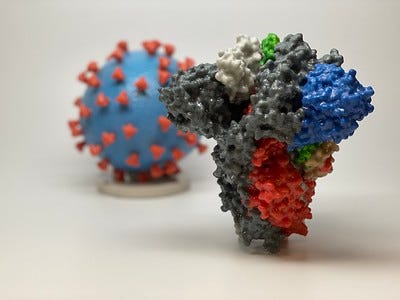
SARS-CoV-2 Protein Structure
Nucleocapsid (N) Proteins are proteins which encapsulate the SARS-CoV-2 viral RNA.
Spike (S) Proteins are complexes of 2 subunits, S1 and S2. They are displayed on the outer portions of the SAR-CoV-2 virus.
S1 is the outer region of the spike protein, which in SARS-CoV-2 can bind with our cells ACE2 receptors. S1 falls away after binding, exposing S2.
S2 is the inner region of the spike protein. Its base is attached to the SAR-CoV-2 virus particle. If it is exposed by S1 falling away, it changes shape twice. S1 first stretches out and attaches to the nearby cell, then contracts and joins the viral particle and cell together.
Amyloidosis Associated Issues
Clotting
Vendruscolo M, Knowles TP, Dobson CM. Protein solubility and protein homeostasis: a generic view of protein misfolding disorders. Cold Spring Harb Perspect Biol. 2011 Dec 1;3(12):a010454. doi: 10.1101/cshperspect.a010454. PMID: 21825020; PMCID: PMC3225949.
Cortes-Canteli M, Paul J, Norris EH, Bronstein R, Ahn HJ, Zamolodchikov D, Bhuvanendran S, Fenz KM, Strickland S. Fibrinogen and beta-amyloid association alters thrombosis and fibrinolysis: a possible contributing factor to Alzheimer's disease. Neuron. 2010 Jun 10;66(5):695-709. doi: 10.1016/j.neuron.2010.05.014. PMID: 20547128; PMCID: PMC2895773.
Taste Loss
Ujike H, Yamamoto M, Hara I. Taste loss as an initial symptom of primary amyloidosis. J Neurol Neurosurg Psychiatry. 1987 Jan;50(1):111-2. doi: 10.1136/jnnp.50.1.111. PMID: 3819746; PMCID: PMC1033269.
Marinone MG, Marinone MG, Merlini G. Reduced taste perception in AL amyloidosis. A frequently unnoticed sensory impairment. Haematologica. 1996 Mar-Apr;81(2):110-5. PMID: 8641637.
Myocarditis
Bois MC, Boire NA, Layman AJ, Aubry MC, Alexander MP, Roden AC, Hagen CE, Quinton RA, Larsen C, Erben Y, Majumdar R, Jenkins SM, Kipp BR, Lin PT, Maleszewski JJ. COVID-19-Associated Nonocclusive Fibrin Microthrombi in the Heart. Circulation. 2021 Jan 19;143(3):230-243. doi: 10.1161/CIRCULATIONAHA.120.050754. Epub 2020 Nov 16. PMID: 33197204; PMCID: PMC7805556.
Lim HE, Pak HN, Kim YH. Acute myocarditis associated with cardiac amyloidosis manifesting as transient complete atrioventricular block and slow ventricular tachycardia. Int J Cardiol. 2006 May 24;109(3):395-7. doi: 10.1016/j.ijcard.2005.05.043. Epub 2005 Jun 17. PMID: 15964086.
Ground Glass Lung Images
Czeyda-Pommersheim F, Hwang M, Chen SS, Strollo D, Fuhrman C, Bhalla S. Amyloidosis: Modern Cross-sectional Imaging. Radiographics. 2015 Sep-Oct;35(5):1381-92. doi: 10.1148/rg.2015140179. Epub 2015 Jul 31. PMID: 26230754.
Pickford HA, Swensen SJ, Utz JP. Thoracic cross-sectional imaging of amyloidosis. AJR Am J Roentgenol. 1997 Feb;168(2):351-5. doi: 10.2214/ajr.168.2.9016204. PMID: 9016204.
Guillain-Barré
Lingenfelser T, Linke RP, Dette S, Roggendorf W, Wiethölter H. AL amyloidosis mimicking a preferentially autonomic chronic Guillain-Barré syndrome. Clin Investig. 1992 Feb;70(2):159-62. doi: 10.1007/BF00227360. PMID: 1600343.
Hu D, Liu L, Yuan S, Yi Y, Peng D. Familial amyloid cardiomyopathy masquerading as chronic Guillain-Barre syndrome: things are not always what they seem. Front Med. 2017 Jun;11(2):293-296. doi: 10.1007/s11684-017-0516-9. Epub 2017 Apr 19. PMID: 28425041.
Bell's Palsy / Facial Paralysis
Martins AM, Ferreira FS, Leite IM, Fonseca M, Victorino R. Facial Paralysis as Initial Manifestation of Light-chain Amyloidosis. Cureus. 2019 Aug 29;11(8):e5521. doi: 10.7759/cureus.5521. PMID: 31687296; PMCID: PMC6819054.
Ruiz-Laiglesia FJ, Pérez-Calvo JI, Torrubia-Pérez CB, Castiella-Muruzabal T, Morandeira-García MJ. Liver Failure and Peripheral Facial Paralysis in a Case of Primary Amyloidosis. Arch Intern Med. 1998;158(18):2066–2067. doi:
Stroke
Charidimou A, Boulouis G, Gurol ME, Ayata C, Bacskai BJ, Frosch MP, Viswanathan A, Greenberg SM. Emerging concepts in sporadic cerebral amyloid angiopathy. Brain. 2017 Jul 1;140(7):1829-1850. doi: 10.1093/brain/awx047. PMID: 28334869; PMCID: PMC6059159.
Li Q, Yang Y, Reis C, Tao T, Li W, Li X, Zhang JH. Cerebral Small Vessel Disease. Cell Transplant. 2018 Dec;27(12):1711-1722. doi: 10.1177/0963689718795148. Epub 2018 Sep 25. PMID: 30251566; PMCID: PMC6300773.
Postural Orthostatic Tachycardia Syndrome (POTS)
Eldokla AM, Numan MT. Postural orthostatic tachycardia syndrome after mRNA COVID-19 vaccine. Clin Auton Res. 2022 Aug;32(4):307-311. doi: 10.1007/s10286-022-00880-3. Epub 2022 Jul 23. PMID: 35870086; PMCID: PMC9308031.
Agarwal AK, Garg R, Ritch A, Sarkar P. Postural orthostatic tachycardia syndrome. Postgrad Med J. 2007 Jul;83(981):478-80. doi: 10.1136/pgmj.2006.055046. PMID: 17621618; PMCID: PMC2600095.
Grubb BP. Postural tachycardia syndrome. Circulation. 2008 May 27;117(21):2814-7. doi: 10.1161/CIRCULATIONAHA.107.761643. PMID: 18506020.
Heart Failure
Garcia-Pavia P, Rapezzi C, Adler Y, Arad M, Basso C, Brucato A, Burazor I, Caforio ALP, Damy T, Eriksson U, Fontana M, Gillmore JD, Gonzalez-Lopez E, Grogan M, Heymans S, Imazio M, Kindermann I, Kristen AV, Maurer MS, Merlini G, Pantazis A, Pankuweit S, Rigopoulos AG, Linhart A. Diagnosis and treatment of cardiac amyloidosis: a position statement of the ESC Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2021 Apr 21;42(16):1554-1568. doi: 10.1093/eurheartj/ehab072. PMID: 33825853; PMCID: PMC8060056.
Mohty D, Damy T, Cosnay P, Echahidi N, Casset-Senon D, Virot P, Jaccard A. Cardiac amyloidosis: updates in diagnosis and management. Arch Cardiovasc Dis. 2013 Oct;106(10):528-40. doi: 10.1016/j.acvd.2013.06.051. Epub 2013 Sep 23. PMID: 24070600.
Platelet Activation
Herczenik E, Bouma B, Korporaal SJ, Strangi R, Zeng Q, Gros P, Van Eck M, Van Berkel TJ, Gebbink MF, Akkerman JW. Activation of human platelets by misfolded proteins. Arterioscler Thromb Vasc Biol. 2007 Jul;27(7):1657-65. doi: 10.1161/ATVBAHA.107.143479. Epub 2007 May 17. PMID: 17510465.
Pielsticker C, Brodde MF, Raum L, Jurk K, Kehrel BE. Plasmin-Induced Activation of Human Platelets Is Modulated by Thrombospondin-1, Bona Fide Misfolded Proteins and Thiol Isomerases. Int J Mol Sci. 2020 Nov 23;21(22):8851. doi: 10.3390/ijms21228851. PMID: 33238433; PMCID: PMC7700677.
Encephalitis
Kloppenborg, R.P., Richard, E., Sprengers, M.E. et al. Steroid responsive encephalopathy in cerebral amyloid angiopathy: a case report and review of evidence for immunosuppressive treatment. J Neuroinflammation 7, 18 (2010). https://doi.org/10.1186/1742-2094-7-18
Grasso D, Castorani G, Borreggine C, Simeone A, De Blasi R. Cerebral amyloid angiopathy related inflammation: A little known but not to be underestimated disease. Radiol Case Rep. 2021 Jul 3;16(9):2514-2521. doi: 10.1016/j.radcr.2021.05.080. PMID: 34257791; PMCID: PMC8260958.
Skin Problems
Freeman R, Gonzalez-Duarte A, Barroso F, Campagnolo M, Rajan S, Garcia J, Kim JY, Wang N, Orellana L, Gibbons C. Cutaneous amyloid is a biomarker in early ATTRv neuropathy and progresses across disease stages. Ann Clin Transl Neurol. 2022 Sep;9(9):1370-1383. doi: 10.1002/acn3.51636. Epub 2022 Aug 9. PMID: 35945901; PMCID: PMC9463946.
Atzori L, Ferreli C, Matucci-Cerinic C, Pilloni L, Rongioletti F. Primary Localized Cutaneous Nodular Amyloidosis and Limited Cutaneous Systemic Sclerosis: Additional Cases with Dermatoscopic and Histopathological Correlation of Amyloid Deposition. Dermatopathology (Basel). 2021 Jul 2;8(3):229-235. doi: 10.3390/dermatopathology8030028. PMID: 34287266; PMCID: PMC8293241.
Tunneling Nanotubes are Associated with Amyloids
Scientific American: COVID Virus May Tunnel through Nanotubes from Nose to Brain
Pepe A, Pietropaoli S, Vos M, Barba-Spaeth G, Zurzolo C. Tunneling nanotubes provide a route for SARS-CoV-2 spreading. Sci Adv. 2022 Jul 22;8(29):eabo0171. doi: 10.1126/sciadv.abo0171. Epub 2022 Jul 20. PMID: 35857849; PMCID: PMC9299553.
Cordero Cervantes D, Zurzolo C. Peering into tunneling nanotubes-The path forward. EMBO J. 2021 Apr 15;40(8):e105789. doi: 10.15252/embj.2020105789. Epub 2021 Mar 1. PMID: 33646572; PMCID: PMC8047439.
Dilna A, Deepak KV, Damodaran N, Kielkopf CS, Kagedal K, Ollinger K, Nath S. Amyloid-β induced membrane damage instigates tunneling nanotube-like conduits by p21-activated kinase dependent actin remodulation. Biochim Biophys Acta Mol Basis Dis. 2021 Dec 1;1867(12):166246. doi: 10.1016/j.bbadis.2021.166246. Epub 2021 Aug 15. PMID: 34403739.
Diabetes is Associated with Misfolded Proteins
Scheuner D, Kaufman RJ. The unfolded protein response: a pathway that links insulin demand with beta-cell failure and diabetes. Endocr Rev. 2008 May;29(3):317-33. doi: 10.1210/er.2007-0039. Epub 2008 Apr 24. Erratum in: Endocr Rev. 2008 Aug;29(5):631. PMID: 18436705; PMCID: PMC2528859.
Iwawaki T, Oikawa D. The role of the unfolded protein response in diabetes mellitus. Semin Immunopathol. 2013 May;35(3):333-50. doi: 10.1007/s00281-013-0369-5. Epub 2013 Mar 26. PMID: 23529219.
Articles Mentioning Amyloids and COVID
Nature: Could tiny blood clots cause long COVID’s puzzling symptoms?
Mayo Clinic: Blood clots in the heart are common in patients with COVID-19
Science Daily: Possible discovery of mechanism behind mysterious COVID-19 symptoms
Medical News Today: Misfolded spike protein could explain complicated COVID-19 symptoms
Hematology Advisor: Are Amyloid Fibrin Microclots Central to Long COVID?
News-Medical.net: Can SARS-CoV-2 trigger amyloidosis?
News-Medical.net: A possible link between aggregation of SARS-CoV-2 proteins and protein misfolding diseases
Link to 3D animation of amyloidosis structure and mechanism:
Excellent in-depth structural overview of amyloids:
Willbold D, Strodel B, Schröder GF, Hoyer W, Heise H. Amyloid-type Protein Aggregation and Prion-like Properties of Amyloids. Chem Rev. 2021 Jul 14;121(13):8285-8307. doi: 10.1021/acs.chemrev.1c00196. Epub 2021 Jun 17. PMID: 34137605.
*This post is likely to be updated after publishing. I will try to include any additional relevant information and remove any false information, so that it can be referenced.
Sinha N, Thakur AK. Likelihood of amyloid formation in COVID-19-induced ARDS. Trends Microbiol. 2021 Nov;29(11):967-969. doi: 10.1016/j.tim.2021.03.008. Epub 2021 Mar 29. PMID: 33795156; PMCID: PMC8007089.
Gonçalves CA, Bobermin LD, Sesterheim P, Netto CA. SARS-CoV-2-Induced Amyloidgenesis: Not One, but Three Hypotheses for Cerebral COVID-19 Outcomes. Metabolites. 2022 Nov 11;12(11):1099. doi: 10.3390/metabo12111099. PMID: 36422238; PMCID: PMC9692683.
Semerdzhiev SA, Fakhree MAA, Segers-Nolten I, Blum C, Claessens MMAE. Interactions between SARS-CoV-2 N-Protein and α-Synuclein Accelerate Amyloid Formation. ACS Chem Neurosci. 2022 Jan 5;13(1):143-150. doi: 10.1021/acschemneuro.1c00666. Epub 2021 Dec 3. PMID: 34860005; PMCID: PMC8739828.
Galkin AP. Hypothesis: AA amyloidosis is a factor causing systemic complications after coronavirus disease. Prion. 2021 Dec;15(1):53-55. doi: 10.1080/19336896.2021.1910468. PMID: 33876719; PMCID: PMC8078534.
Russe-Russe JR, Abramowitz C, Pellegrini JR, Alvarez Betancourt A, Cohen R, Baldino M, Crandall R, Kagolanu D, Mejia J, Rizvon K. COVID-19 Exposure Unmasking Systemic Amyloidosis With Hepatic Predominance. Cureus. 2022 Nov 4;14(11):e31092. doi: 10.7759/cureus.31092. PMID: 36475164; PMCID: PMC9719725.
Grobbelaar LM, Venter C, Vlok M, Ngoepe M, Laubscher GJ, Lourens PJ, Steenkamp J, Kell DB, Pretorius E. SARS-CoV-2 spike protein S1 induces fibrin(ogen) resistant to fibrinolysis: implications for microclot formation in COVID-19. Biosci Rep. 2021 Aug 27;41(8):BSR20210611. doi: 10.1042/BSR20210611. PMID: 34328172; PMCID: PMC8380922.
Li Y, Lu S, Gu J, Xia W, Zhang S, Zhang S, Wang Y, Zhang C, Sun Y, Lei J, Liu C, Su Z, Yang J, Peng X, Li D. SARS-CoV-2 impairs the disassembly of stress granules and promotes ALS-associated amyloid aggregation. Protein Cell. 2022 Aug;13(8):602-614. doi: 10.1007/s13238-022-00905-7. Epub 2022 Apr 6. PMID: 35384603; PMCID: PMC8983322.
Bhardwaj T, Gadhave K, Kapuganti SK, Kumar P, Brotzakis ZF, Saumya KU, Nayak N, Kumar A, Joshi R, Mukherjee B, Bhardwaj A, Thakur KG, Garg N, Vendruscolo M, Giri R. Amyloidogenic proteins in the SARS-CoV and SARS-CoV-2 proteomes. Nat Commun. 2023 Feb 20;14(1):945. doi: 10.1038/s41467-023-36234-4. PMID: 36806058; PMCID: PMC9940680.
Angammana C, Gamlath S, Karunathilake R, Silva S. Tracheobronchial amyloidosis following COVID-19 infection. Respirol Case Rep. 2024 Dec 3;12(12):e70073. doi: 10.1002/rcr2.70073. PMID: 39629258; PMCID: PMC11614462.
Nyström S, Hammarström P. Amyloidogenesis of SARS-CoV-2 Spike Protein. J Am Chem Soc. 2022 May 25;144(20):8945-8950. doi: 10.1021/jacs.2c03925. Epub 2022 May 17. PMID: 35579205; PMCID: PMC9136918.
Seth P, Sarkar N. A comprehensive mini-review on amyloidogenesis of different SARS-CoV-2 proteins and its effect on amyloid formation in various host proteins. 3 Biotech. 2022 Nov;12(11):322. doi: 10.1007/s13205-022-03390-1. Epub 2022 Oct 13. PMID: 36254263; PMCID: PMC9558030.
Aksenova AY, Likhachev IV, Grishin SY, Galzitskaya OV. The Increased Amyloidogenicity of Spike RBD and pH-Dependent Binding to ACE2 May Contribute to the Transmissibility and Pathogenic Properties of SARS-CoV-2 Omicron as Suggested by In Silico Study. Int J Mol Sci. 2022 Nov 4;23(21):13502. doi: 10.3390/ijms232113502. PMID: 36362302; PMCID: PMC9655063.
Petrlova J, Samsudin F, Bond PJ, Schmidtchen A. SARS-CoV-2 spike protein aggregation is triggered by bacterial lipopolysaccharide. FEBS Lett. 2022 Oct;596(19):2566-2575. doi: 10.1002/1873-3468.14490. Epub 2022 Sep 11. PMID: 36050806; PMCID: PMC9538650.
Petrovszki D, Walter FR, Vigh JP, Kocsis A, Valkai S, Deli MA, Dér A. Penetration of the SARS-CoV-2 Spike Protein across the Blood-Brain Barrier, as Revealed by a Combination of a Human Cell Culture Model System and Optical Biosensing. Biomedicines. 2022 Jan 17;10(1):188. doi: 10.3390/biomedicines10010188. PMID: 35052867; PMCID: PMC8773803.
Rhea EM, Logsdon AF, Hansen KM, Williams LM, Reed MJ, Baumann KK, Holden SJ, Raber J, Banks WA, Erickson MA. The S1 protein of SARS-CoV-2 crosses the blood-brain barrier in mice. Nat Neurosci. 2021 Mar;24(3):368-378. doi: 10.1038/s41593-020-00771-8. Epub 2020 Dec 16. PMID: 33328624; PMCID: PMC8793077.
Mörz M. A Case Report: Multifocal Necrotizing Encephalitis and Myocarditis after BNT162b2 mRNA Vaccination against COVID-19. Vaccines (Basel). 2022 Oct 1;10(10):1651. doi: 10.3390/vaccines10101651. PMID: 36298516; PMCID: PMC9611676.
Rong Z, Mai H, Ebert G, Kapoor S, Puelles VG, Czogalla J, Hu S, Su J, Prtvar D, Singh I, Schädler J, Delbridge C, Steinke H, Frenzel H, Schmidt K, Braun C, Bruch G, Ruf V, Ali M, Sühs KW, Nemati M, Hopfner F, Ulukaya S, Jeridi D, Mistretta D, Caliskan ÖS, Wettengel JM, Cherif F, Kolabas ZI, Molbay M, Horvath I, Zhao S, Krahmer N, Yildirim AÖ, Ussar S, Herms J, Huber TB, Tahirovic S, Schwarzmaier SM, Plesnila N, Höglinger G, Ondruschka B, Bechmann I, Protzer U, Elsner M, Bhatia HS, Hellal F, Ertürk A. Persistence of spike protein at the skull-meninges-brain axis may contribute to the neurological sequelae of COVID-19. Cell Host Microbe. 2024 Nov 26:S1931-3128(24)00438-4. doi: 10.1016/j.chom.2024.11.007. Epub ahead of print. PMID: 39615487.
Idrees D, Kumar V. SARS-CoV-2 spike protein interactions with amyloidogenic proteins: Potential clues to neurodegeneration. Biochem Biophys Res Commun. 2021 May 21;554:94-98. doi: 10.1016/j.bbrc.2021.03.100. Epub 2021 Mar 24. PMID: 33789211; PMCID: PMC7988450.
Ma, G., Zhang, DF., Zou, QC. et al. SARS-CoV-2 Spike protein S2 subunit modulates γ-secretase and enhances amyloid-β production in COVID-19 neuropathy. Cell Discov 8, 99 (2022). https://doi.org/10.1038/s41421-022-00458-3
Charnley, M., Islam, S., Bindra, G.K. et al. Neurotoxic amyloidogenic peptides in the proteome of SARS-COV2: potential implications for neurological symptoms in COVID-19. Nat Commun 13, 3387 (2022). https://doi.org/10.1038/s41467-022-30932-1
Ferrucci R, Cuffaro L, Capozza A, Rosci C, Maiorana N, Groppo E, Reitano MR, Poletti B, Ticozzi N, Tagliabue L, Silani V, Priori A. Brain positron emission tomography (PET) and cognitive abnormalities one year after COVID-19. J Neurol. 2023 Jan 24:1–12. doi: 10.1007/s00415-022-11543-8. Epub ahead of print. PMID: 36692636; PMCID: PMC9873215.
Priemer DS, Rhodes CH, Karlovich E, Perl DP, Goldman JE. Aβ Deposits in the Neocortex of Adult and Infant Hypoxic Brains, Including in Cases of COVID-19. J Neuropathol Exp Neurol. 2022 Nov 16;81(12):988-995. doi: 10.1093/jnen/nlac095. PMID: 36264253.
Liang HW, Mung SM, Douglass C, Jude EB. COVID-19-related vasculopathy of the brain. BMJ Case Rep. 2021 Jul 27;14(7):e242028. doi: 10.1136/bcr-2021-242028. PMID: 34315736; PMCID: PMC8316986.
Ziff OJ, Ashton NJ, Mehta PR, Brown R, Athauda D, Heaney J, Heslegrave AJ, Benedet AL, Blennow K, Checkley AM, Houlihan CF, Gauthier S, Rosa-Neto P, Fox NC, Schott JM, Zetterberg H, Benjamin LA, Paterson RW. Amyloid processing in COVID-19-associated neurological syndromes. J Neurochem. 2022 Apr;161(2):146-157. doi: 10.1111/jnc.15585. Epub 2022 Mar 2. PMID: 35137414; PMCID: PMC9115071.
Shen WB, Elahi M, Logue J, Yang P, Baracco L, Reece EA, Wang B, Li L, Blanchard TG, Han Z, Rissman RA, Frieman MB, Yang P. SARS-CoV-2 invades cognitive centers of the brain and induces Alzheimer's-like neuropathology. bioRxiv [Preprint]. 2022 Sep 6:2022.01.31.478476. doi: 10.1101/2022.01.31.478476. PMID: 35132414; PMCID: PMC8820661.
Pretorius E, Venter C, Laubscher GJ, Kotze MJ, Oladejo SO, Watson LR, Rajaratnam K, Watson BW, Kell DB. Prevalence of symptoms, comorbidities, fibrin amyloid microclots and platelet pathology in individuals with Long COVID/Post-Acute Sequelae of COVID-19 (PASC). Cardiovasc Diabetol. 2022 Aug 6;21(1):148. doi: 10.1186/s12933-022-01579-5. PMID: 35933347; PMCID: PMC9356426.
Pretorius E, Venter C, Laubscher GJ, Lourens PJ, Steenkamp J, Kell DB. Prevalence of readily detected amyloid blood clots in 'unclotted' Type 2 Diabetes Mellitus and COVID-19 plasma: a preliminary report. Cardiovasc Diabetol. 2020 Nov 17;19(1):193. doi: 10.1186/s12933-020-01165-7. PMID: 33203441; PMCID: PMC7670290.
Pretorius, Etheresia & Venter, Chantelle & Laubshder, Gert & Kotze, Maritha & Moremi, Kelebogile & Oladejo, Sunday & Watson, Liam & Rajaratnam, Kanshukan & Kell, Douglas. (2021). Combined triple treatment of fibrin amyloid microclots and platelet pathology in individuals with Long COVID/ Post-Acute Sequelae of COVID-19 (PASC) can resolve their persistent symptoms. 10.21203/rs.3.rs-1205453/v1.
Kruger A, Vlok M, Turner S, Venter C, Laubscher GJ, Kell DB, Pretorius E. Proteomics of fibrin amyloid microclots in long COVID/post-acute sequelae of COVID-19 (PASC) shows many entrapped pro-inflammatory molecules that may also contribute to a failed fibrinolytic system. Cardiovasc Diabetol. 2022 Sep 21;21(1):190. doi: 10.1186/s12933-022-01623-4. PMID: 36131342; PMCID: PMC9491257.
Kell DB, Laubscher GJ, Pretorius E. A central role for amyloid fibrin microclots in long COVID/PASC: origins and therapeutic implications. Biochem J. 2022 Feb 17;479(4):537-559. doi: 10.1042/BCJ20220016. PMID: 35195253; PMCID: PMC8883497.
Perez, J.-C., Moret-Chalmin, C., & Montagnier, L. (2023). Emergence of a New Creutzfeldt-Jakob Disease: 26 Cases of the Human Version of Mad-Cow Disease, Days After a COVID-19 Injection. International Journal of Vaccine Theory, Practice, and Research, 3(1), 727–770. Retrieved from https://ijvtpr.com/index.php/IJVTPR/article/view/66
Tetz G, Tetz V. Prion-like Domains in Spike Protein of SARS-CoV-2 Differ across Its Variants and Enable Changes in Affinity to ACE2. Microorganisms. 2022 Jan 25;10(2):280. doi: 10.3390/microorganisms10020280. PMID: 35208734; PMCID: PMC8878784.
Zhao Y, Jaber VR, Lukiw WJ. SARS-CoV-2, long COVID, prion disease and neurodegeneration. Front Neurosci. 2022 Sep 27;16:1002770. doi: 10.3389/fnins.2022.1002770. PMID: 36238082; PMCID: PMC9551214.
Baazaoui N, Iqbal K. COVID-19 and Neurodegenerative Diseases: Prion-Like Spread and Long-Term Consequences. J Alzheimers Dis. 2022;88(2):399-416. doi: 10.3233/JAD-220105. PMID: 35599487.
Actis GC, Ribaldone DG, Pellicano R. COVID vaccine's hot problems: erratic serious blood clotting, ill-defined prion-like reactogenicity of the spike, unclear roles of other factors. Minerva Med. 2021 Dec;112(6):695-697. doi: 10.23736/S0026-4806.21.07769-7. PMID: 35168305.
Shahzad, S., Willcox, M. The Possible Role of Prion-Like Viral Protein Domains on the Emergence of Novel Viruses as SARS-CoV-2. J Mol Evol 90, 227–230 (2022). https://doi.org/10.1007/s00239-022-10054-4
Seneff S, Kyriakopoulos AM, Nigh G, McCullough PA. A Potential Role of the Spike Protein in Neurodegenerative Diseases: A Narrative Review. Cureus. 2023 Feb 11;15(2):e34872. doi: 10.7759/cureus.34872. PMID: 36788995; PMCID: PMC9922164.
Laudicella R, Burger IA, Panasiti F, Longo C, Scalisi S, Minutoli F, Baldari S, Grimaldi LME, Alongi P. Subcutaneous Uptake on [18F]Florbetaben PET/CT: a Case Report of Possible Amyloid-Beta Immune-Reactivity After COVID-19 Vaccination. SN Compr Clin Med. 2021;3(12):2626-2628. doi: 10.1007/s42399-021-01058-0. Epub 2021 Sep 14. PMID: 34541458; PMCID: PMC8439537.



Great compilation of research, so helpful to have it all in one place instead of having to hunt all my bookmarks for the papers xoxo!! You have my eternal gratitude.
Http://dbkgroup.org/longcovid/ explains